Boeing and Kratos TDI sign MoU on Powered JDAM munition - Airforce Technology
The integration of an engine into the existing JDAM kit will provide increased range for 500lb air-released munitions.
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.



Pahempi joukkoammuskelu Mainessa. Papparainen lupasi tehdä kaikkensa näiden estämiseksi mutta päinvastoin ampumisia lienee enemmän kuin koskaan ennen.
Kuvassa näkyy valkoihoinen ampuja joten kyseessä lienee trumpisti.

Toistakymmentä kuollut joukkoampumisessa Yhdysvalloissa – ampuja edelleen vapaana
Epäilty ampuja on 40-vuotias mies. Poliisin mukaan hän on aseistettu ja vaarallinen.www.is.fi
Poliisi on kertonut etsivänsä ”tapaukseen liittyen” henkilöä nimeltä Robert Card. Viranomaiset varoittavat Cardin olevan aseistautunut ja vaarallinen.
Viranomaisille tarkoitetun tietokannan mukaan 40-vuotias Card on ampuma-asekouluttaja, jonka uskotaan olleen armeijan reservissä, kertoo NBC News. Tiedotteen mukaan Card oli vastikään kertonut mielenterveysongelmista. https://www.iltalehti.fi/ulkomaat/a/2faafbf6-7e78-44b5-b882-94ad835364c6
Card, who is twice divorced and a father of three children, has a history of arrests for domestic violence and other crimes. One of his ex-wives obtained a restraining order against him.
While Card identifies as an independent politically, reports suggest he may have voted for Barack Obama in the past.
There have been no signs of suspicious activity in recent weeks, either in person or on his social media, and there is no record of mental illnesses. https://www.marca.com/en/lifestyle/us-news/2023/10/26/6539d51e22601d92678b457b.html




Johtuukohan hankkeen hitaus siitä, että ohjuksen kehittäminen ei onnistu vaiko siitä, että ohjuksesta ei tule niin hyvä kuin mitä haluttaisiin. Turha tehdä samanlaista ryssittyä mikä ryssillä jo on, kun voi tehdä paremmankin.
USA:n hypersoonisen ohjuksen testi epäonnistui jälleen, ase lykkääntyy hamaan tulevaisuuteen – Venäjällä ja Kiinalla ohjus on jo käytössä
Jostain syytä Yhdysvallat kompuroi asekehityksessä.www.tekniikkatalous.fi
Kun jenkit tekee todellista hypersoonista ohjusta (jos oikein ymmärtänyt), vs ryssän ilmasta laukaistava ballistinen ohjus, voi haasteet olla hieman eri kertaluokassaJohtuukohan hankkeen hitaus siitä, että ohjuksen kehittäminen ei onnistu vaiko siitä, että ohjuksesta ei tule niin hyvä kuin mitä haluttaisiin. Turha tehdä samanlaista ryssittyä mikä ryssillä jo on, kun voi tehdä paremmankin.

“Kinzhal is nothing more than an air-launched ballistic missile,” Jeffrey Lewis, Ph.D., of the James Martin Center for Nonproliferation Studies in Monterey, California, tells Popular Mechanics. “It’s only hypersonic in the sense that pretty much all ballistic missiles are hypersonic.”
Sidharth Kaushal, Ph.D., of the U.K.-based defense think tank RUSI is similarly doubtful about the “hypersonic” label. “It doesn’t meet the maneuverability criteria for being a true hypersonic weapon,” he tells Popular Mechanics.
USA:ssa rahaa riittää, mutta kyllä sitä osataan käyttääkin. USA:ssa käytetään terveydenhuoltoon reilusti eniten rahaa maailmassa per capita. Ja kyllä, siihen käytetään myös julkisia varoja jättimäisesti per capita, mutta julkinen terveydenhuolto kattaa vain pienehkön osan kansasta.Senaattorit Elisabeth Warren(D) ja Mike Brown(R) vaativat terveysministeriötä tutkimaan terveysvakuutusyhtiöiden keinotekoista lääkehintojen kohottamista.
Terveysvakuutusyhtiöt omistavat apteekkeja. Eli he tarkoituksella ostavat ylihintaan lääkkeitä omistamistamistaan apteekeistaan. Sitten ne laskutetaan pahaa aavistamattomilta asikkailta.
Senaattorit perustavat tutkimusvaatimuksensa edellisessä viestissä esitettyyn WSJ:n artikkeliin.
Tämä on iso juttu. Amerikassa terveyskulut ovat lähellä 20% bkt:stä. Meillä taitaa jäädä alle 10% Bkt:stä?
Yleensä Amerikassa näistä tulee kunnon sakot.

Senators Call for Investigation of Health Insurers’ Role in Driving Up Drug Costs
The request follows a Wall Street Journal article reporting that health insurers were paying much more for drugs for cancer and multiple sclerosis than manufacturers charge.www.wsj.com
A pair of U.S. senators called on the federal government to investigate health insurers that are paying high prices for generic drugs for serious diseases like cancer and multiple sclerosis.
Sen. Elizabeth Warren (D., Mass.) and Sen. Mike Braun (R., Ind.) sent a letter on Wednesday to the U.S. Department of Health and Human Services’ Office of Inspector General requesting an investigation into the high drug prices and any role played by health insurers’ shared ownership with the pharmacies that often fill the prescriptions.
The letter cites a recent article in The Wall Street Journal that reported that big health insurers
Cigna Group
,
CVS Health
and
UnitedHealth Group
are paying multiples more for drugs such as cancer therapy Gleevec and multiple-sclerosis treatment Tecfidera than what manufacturers charge for generic versions.
“These findings are alarming,” the senators said of the Journal article in its letter to HHS Inspector General Christi Grimm. “This anticompetitive behavior raises costs, hurts independent pharmacies, and undercuts Congress’ ability to rein in excessive profits of insurance companies.”
Generics are supposed to help health plans keep a lid on drug spending. Healthcare experts say insurers, even though they reimburse pharmacies for drugs, can profit by charging high prices if their parent companies also own pharmacies and other players in the drug-supply chain. That is because insurers often steer patients to use their own pharmacies, keeping the money under the same roof.
Cigna
owns Express Scripts, a pharmacy-benefit manager, or PBM, that negotiates drug prices with pharmaceutical companies, and the specialty pharmacy Accredo. CVS operates the Caremark PBM, as well as health-insurer Aetna and thousands of retail pharmacies.
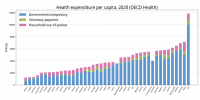



USA:ssa rahaa riittää, mutta kyllä sitä osataan käyttääkin. USA:ssa käytetään terveydenhuoltoon reilusti eniten rahaa maailmassa per capita. Ja kyllä, siihen käytetään myös julkisia varoja jättimäisesti per capita, mutta julkinen terveydenhuolto kattaa vain pienehkön osan kansasta.
Europe is "irrelevant," throwing U.S. weight around in the Caribbean and Latin America is a given, and Americans who oppose him are "confused and frustrated."
So say former President Richard Nixon and his closest confidant, Henry Kissinger, in papers released Monday by the National Archives. Only China's absolutist leaders seemed to win their unmitigated praise.
"We speak to no other country as frankly and openly as we do to you," Kissinger tells Chinese leader Mao Tse-tung in February 1973, a year after Nixon's breakthrough visit to that country.
The latest batch of Nixon papers to reach the public — nearly 110,000 pages — cover mostly national security issues.
They reveal Nixon and Kissinger as a mutually admiring pair whose views of the world veered from dark and pessimistic to clear-eyed and sympathetic — sometimes in the same meeting, sometimes in the same sentence.
Nixon and Kissinger closely cultivate and frequently consult with the United States' NATO allies, assuaging their early 1970s concerns about Soviet expansionism and stroking the egos of European leaders.
"We feel that you should take an active role in world affairs," Nixon tells British Prime Minister Edward Heath in a December 1971 meeting.
Just over a year later, Kissinger offhandedly dismisses the entire continent in a remark to Mao:
"What Europe thinks (of the Soviet Union) I am not able to judge. They cannot do anything anyway. They are basically irrelevant."... jatkuu CBS:n jutussa