Behind the Global Race to Contain China’s Killer Bug
“What we are facing now is an extreme, severe and abrupt public health crisis.”
In early January, doctors in Wuhan, a transportation and tech hub in central China, worked frantically to save the life of a 61-year-old man infected with a new and unknown virus. He checked in with severe pneumonia, on top of his preexisting issues with abdominal tumors and chronic liver disease. Infection-fighting medicines didn’t work. His blood was pumped through an artificial lung, then he went into septic shock and his vital organs shut down. He slipped away on Jan. 9.
This was no ordinary death. His passing was publicly flagged in an official statement posted by Wuhan’s city government and marked the first known fatality from a viral outbreak that has alarmed infectious disease experts worldwide since news of the illness surfaced in late December.
As January draws to a close, the virus, a strain of the coronavirus family of pathogens, has spread to
four continents. President Xi Jinping’s government has cordoned off much of the central Chinese province of Hubei, practically blockading more than 50 million people, in the biggest large-scale quarantine in the modern era. The Politburo Standing Committee, the nation’s top decision making body, has taken charge of the crisis, appointing a special team to oversee everything from organizing medical care to scientific research in a bid to control an epidemic that’s killed at least 80 people and sickened more than 2,700 worldwide.
Wuhan Hygiene Emergency Response Team staff leave the closed Huanan Seafood Wholesale Market in Wuhan on Jan. 11.
Photographer: Noel Celis/AFP via Getty Images
In Wuhan, the epicenter of the crisis, chaos has taken hold as local hospitals face a patient onslaught and have run short of protective gear, masks and goggles. The city said Friday it would build and open a 1,000-bed specialist hospital for infected patients within 10 days. President Xi called the crisis a “grave situation.”
Beijing has dispatched military doctors to hard-hit locales. “What we are facing now is an extreme, severe and abrupt public health crisis,” Hu Yinghai, deputy head of the civil affairs office of Hubei province, of which Wuhan is the capital, told reporters on Saturday. “Medical goods and materials are in critically short supply.”

A new ban on private car use imposed midnight Saturday had citizens wondering how they’d get to work or buy necessities at the supermarket. “A week ago people were still preparing for the New Year and the government didn’t announce any bans or emergencies then,” said Wuhan resident Wang Jin, 37. “All of a sudden everything changed and they paralyzed the city. It seems to me there must be missed opportunities to contain the disease in an earlier stage.”
Rewind the last five weeks of the China virus outbreak, and you’ll find a tale of bureaucratic miscues, a health-care system unequipped for sudden crises and a food industry in dire need of reform—a public health risk to China and beyond. It’s also a story of individual Chinese caught up in a rapidly changing epidemic and public health professionals, in China and around the world, racing to stay a step ahead of a dangerous and mutating virus.
The viral outbreak last month couldn’t have been more ill-timed, given the approaching Lunar New Year holidays that kicked off on Friday, an epic travel period in greater China and the largest annual human migration in the world. And the government’s early response to the unfolding crisis is getting mixed reviews. While the World Health Organization has praised China for its openness in sharing information, some infectious disease specialists believe local authorities were too slow to contain the outbreak in December and early January.
Travelers wear protective masks while waiting for transport at Hongqiao high-speed railway station before Lunar New Year in Shanghai on Jan. 22.
Photographer: Qilai Shen/Bloomberg
From the start, experts worried about the potential for the virus to mutate, enabling easier spread of the contagion for which there is no effective treatment or vaccine. Even a less-deadly pathogen that’s capable of spreading unchecked could disrupt global public health systems, cause economic losses and further
rattle global markets.
Chinese authorities have already reported “fourth-generation cases,” in which sick individuals have set off a chain reaction that infects three others, and human-to-human transmission has occurred
outside China, according to the WHO.
The anonymous, elderly Chinese who died in early January frequented the popular Huanan Seafood Wholesale Market, a traditional “
wet market” where crowds of shoppers, freshly slaughtered and unwrapped meat and live animals commingle in close quarters. Hens stuffed in metal cages and snakes wriggling in plastic buckets, often sitting alongside garbage and rotten food, are common sights in such markets across China. They also create an ideal breeding ground for dangerous pathogens. (China on Sunday announced a
ban on wildlife trade across the country).
By Jan. 7, Chinese scientists had isolated a novel virus, and its genetic sequence was submitted days later to several online data-sharing portals where public health specialists swap information.
Workers driving excavators at the construction site of a field hospital in Wuhan on Jan. 24.
Source: Stringer/Getty Images
Coronaviruses are known for infecting primarily bats, pigs and other animals and also for their ability to migrate from animals to humans—and also from one human to another. They come in multiple strains, ranging in severity from the common cold to some of the most lethal infections threatening humans, such as severe acute respiratory syndrome, or SARS, and Middle East respiratory syndrome, known as MERS. The Wuhan variety, which the WHO refers to as 2019-nCoV, appears less virulent than SARS at the moment, and most life-threatening to the ill and elderly.
Yet even as the death toll remained relatively low early on, less than a dozen by mid-January, there was reason for concern. Coronaviruses, named for crown-like spikes on their surfaces, can mutate readily after jumping to human hosts.
Richard Hatchett, chief executive officer of the Oslo-based Coalition for Epidemic Preparedness Innovations, pointed to the 1918 influenza pandemic that had a case-fatality ratio of less than 5% but infected up to a third of the world’s population. The vast majority of people who got sick just had the flu, he said. However, ultimately an estimated 50 million people died because it was so widespread.
“That’s the anxiety for everyone in the field, the scenario that plays out in their minds when they encounter a virus that’s behaving like this one,” Hatchett said. “You don’t know which direction things are going to go.”
Weighing on the minds of Chinese officials early in the crisis was the reputational hit the country took during the SARS outbreak, an airborne virus that began in late 2002 in the southern Guangdong province, then quickly spread across the border to Hong Kong and to other Asian countries.
Many of China’s top doctors initially concluded they were dealing with pneumonia caused by chlamydia, a sexually transmissible bacterium. Chinese health minister Zhang Wenkang eventually lost his job for mishandling that crisis, which killed
774 people from China to Canada and led to $40 billion in global economic losses in 2003.
A customer holds face masks at a pharmacy in Hong Kong on Jan. 23.
Photographer: Justin Chin/Bloomberg
Weeks ago, one of the frontline public health experts of that era worried China may have blundered again. Guan Yi is a blunt-talking virologist and director of the State Key Laboratory of Emerging Infectious Diseases at the University of Hong Kong, and something of a celebrity among microbiologists worldwide. Time magazine featured him as one of its 18 “Global Health Heroes” of 2005.
During the darkest days of the SARS crisis, he made the discovery that civet cats—small, sleek nocturnal mammals that serve as the main ingredient in the exotic wildlife dish “
dragon-tiger-phoenix soup”—were probably spreading the SARS virus to human beings. Guan formulated his hypothesis just as SARS was beginning to return in Guangdong at the start of 2004 and may have saved lives with his research.
Guan has been strident in his criticism of Wuhan authorities waiting until Jan. 23 to impose a travel ban—when cases had turned up across many parts of China. A faster response would have enabled officials to curb the movement of people who were still in the incubation phase and prevent virus-carriers from transporting it outside the flourishing mega-city.
A notice offering guidance to travelers from Wuhan is displayed as passengers pass through a quarantine station at Narita Airport in Japan on Jan. 23.
Photographer: Kiyoshi Ota/Bloomberg
After returning from a short trip to Wuhan in mid-January and based on his own estimates, he predicted that this latest epidemic “could end up at least 10 times the scale of SARS,” he said in an interview with Caixin magazine.
Neil Ferguson, a researcher at Imperial College London, calculated the number of infected people is much higher than official figures, estimating 4,000 cases in Wuhan as of Jan. 18. The total could have been as high as 9,700 by then, he said in a
report.
Developments turned worrisome in late January, when the mayor of Wuhan, Zhou Xianwang, claimed a neurosurgical patient’s symptoms were ignored by staff at a medical college hospital, allowing the virus to infect a doctor and 13 patients. That was noticed 7,500 miles (12,000 kilometers) away in Bethesda, Maryland, by Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases. “That made us realize that, similar to SARS, there are some people who are super-spreaders,” he said.
Then there was the dawning possibility that 2019-nCoV had a stealthy quality, at least in its early stages, that may enable it to evade detection by airport thermal scanners at immigration. Fever and other symptoms may not appear for
as many as two weeks after infection.
A staff member screens arriving passengers with thermal scanners at Hankou railway station in Wuhan on Jan. 21.
Source: -/AFP via Getty Images
Doctors described cases among members of a family living in Shenzhen who traveled to Wuhan in late December. Four became infected with the virus, which spread to a fifth person after they returned home on Jan. 4—one of the earliest examples of human-to-human transmission. Two of the confirmed cases had no fever when they were checked by doctors in Shenzhen, and a third—a 10-year-old boy—had no symptoms. “These cryptic cases of walking pneumonia might serve as a possible source to propagate the outbreak,” the doctors said in a paper published in the
Lancet.
Half a world away, Nancy Messonnier, director of the U.S. Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases, had been working seven days a week trying to unravel the secrets of the China virus.
CDC officials were initially comforted by the fact that authorities in China were well trained in identifying the source of an emerging outbreak. But Messonnier and her colleagues became concerned when the culprit hadn’t been found days later. “It became clear that this wasn’t a regular disease that we would have heard about, one where first-line diagnostics would be picking it up.”
On Jan. 8, the CDC sent a memo to state health departments nationwide to alert them to the fact that it “thought something unusual was going on and to increase their vigilance.” When scientists published the genetic sequence of the coronavirus, it confirmed the agency’s worst fears.
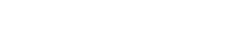
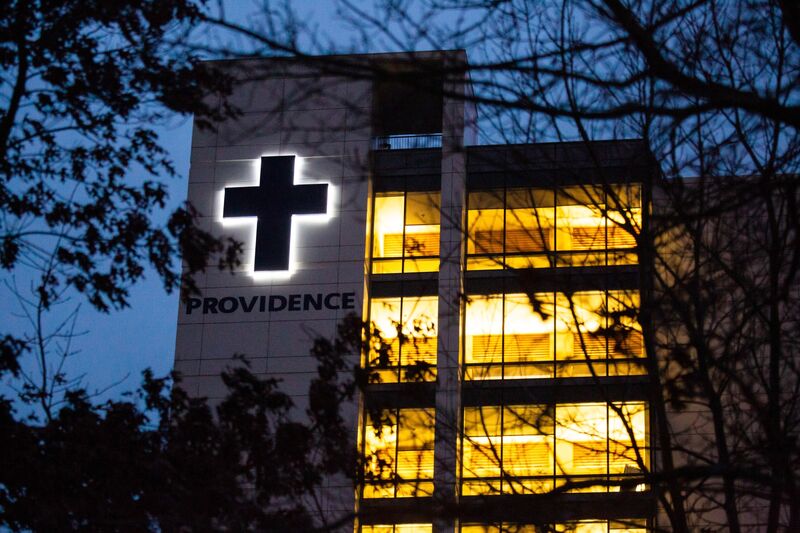
Providence Regional Medical Center is seen in Everett, Washington, on Jan. 21.
Photographer: David Ryder/Bloomberg
Then came the inevitable moment. A 30-something U.S. resident of Snohomish County, Washington, just north of Seattle, returned from a nearly two-month trip to Wuhan on Jan. 15. A day later, he developed mild symptoms, mainly a cough. While he never took his temperature, he was concerned because had heard about the possible outbreak in Wuhan.
He went to a walk-in health clinic on Sunday, Jan. 19, where he showed the clinician information about the outbreak on his phone. The provider immediately called the Washington State Health Department, which called the CDC. The patient was put in protective isolation at Providence Regional Medical Center in Everett, Washington.
While the world’s best disease hunters raced to slow down the advance of the virus, a remarkable human drama was unfolding on the ground in Wuhan, a city of 11 million and, ironically, home to the country’s first maximum biosafety laboratory equipped to study the world’s most dangerous pathogens.
Sometimes called the Chicago of China, Wuhan is an industrial hub along the Yangtze River, just downstream from the massive Three Gorges Dam. Through much of December, local authorities started noticing cases of pneumonia among workers and shoppers of the Huanan Seafood Wholesale Market that were severe enough to warrant hospitalization.
When standard drug treatments didn’t work, and routine tests failed to turn up a likely cause, doctors studied respiratory secretions and other patient specimens to pinpoint the infectious agent. After it appeared to be something similar to SARS, investigators notified municipal, and then provincial, authorities sometime in late December, according to a person familiar with the timeline.
Emergency notices about how to treat a “pneumonia of unknown origin” started to circulate among hospitals. Around that time, China’s National Health Commission dispatched officials to Wuhan to guide the containment strategy. Investigators on Jan. 1 shut down the Wuhan market, where most people infected early in the outbreak either worked or shopped frequently, though cases continued to appear, including in people who hadn’t gone to the market.
Wuhan Hygiene Emergency Response Team staff conduct searches on the closed seafood wholesale market in Wuhan on Jan. 11.
Photographer: Noel Celis/AFP via Getty Images
In early January, it seemed the virus wasn’t transmitted readily between people, reducing the potential of it spawning a SARS-like outbreak. Symptoms varied, with some patients experiencing mainly fever, others fatigue, a dry cough and difficulty breathing.
Other cases were far more extreme. On Jan. 13, Liu Rui, 65, was hospitalized in Tongji Hospital’s fever clinic. All 10 beds were occupied by that point and all the doctors and nurses were wearing protective masks. Yet there was no formal quarantine. Patients, including Liu, came and went as they wished, according to her husband, who declined to be identified by name to protect his privacy.
A day later, a CT scan showed Liu had “white lungs”—the organ’s tiny air sacs were filled with fluid, making it hard for her to breathe. She later slipped into a coma and was put on a ventilator and soon after she passed away.
On Jan. 17, as more ill patients streamed into hospitals, the CDC’s Messonnier told reporters that there
were signs the new pathogen was being transmitted among humans, and not just from animals to humans as was originally hoped. Three days later, Chinese state media also reported health-care workers had been infected—a worrying reminder of the SARS outbreak, in which hospital and clinic workers accounted for almost a quarter of cases.
Nearly a week later, the WHO opted
against designating the outbreak a global health emergency. Yet that hardly mattered back in China, as the government took the extraordinary step of restricting travel in and out of about a dozen cities in central China. It later suspended sales of package tours, and even Shanghai Disneyland temporarily shut down.
Pedestrians wearing protective masks stand in front of a department store on the Nanjing East Road ahead of the Lunar New Year in Shanghai on Jan. 23.
Photographer: Qilai Shen/Bloomberg
Amid the chaos, Luo Jiasi, a 32-year-old Wuhan citizen who works in the new media industry, joined a voluntary group of more than 200 drivers who started transporting medical staff to and from hospitals, as well as gathering donated materials.
“The government certainly has done a lot of work since the epidemic broke out, but there’s a great deal more they can do to improve the situation, like proper disposal of garbage at the wet markets,” Luo said by phone. “Those places could be quite messy with water, decayed food and littering—it’s going to be a hard one to tackle unless we have a garbage sorting system like in Shanghai.”
For ordinary Chinese old enough to remember SARS, and more recent public health scares surrounding outbreaks of avian influenza and swine fever, such sentiments will sound familiar. Nobody in public health can be entirely surprised that China has spawned yet another epidemic, given its population density and food industry practices. The risks from wet markets and China’s spotty record on food safety have been known for decades.
More broadly, though, the emergence and global expansion of 2019-nCoV is a humbling reminder that even in this modern era, with its advances in lifespans, sanitation, vaccination, and antimicrobial therapies, the threat to mankind from infectious diseases is still with us.
— With assistance by Evelyn Yu, Michelle Cortez, Robert Langreth, John Lauerman, James Paton, Lisa Du, Thomas Mulier, Steven Yang, Haze Fan, Dong Lyu, Sarah Chen, Bhuma Shrivastava, Kari Soo Lindberg, and Apple Lam